When living with endometriosis, pain is often a common, frequent symptom. Considered a chronic pain condition, it can have a persistent negative effect on your mental wellbeing. We’ve worked with our mental health counsellor, Ms. Roisin Traynor, to help explain the pain cycle of endometriosis and what she would recommend for coping strategies.
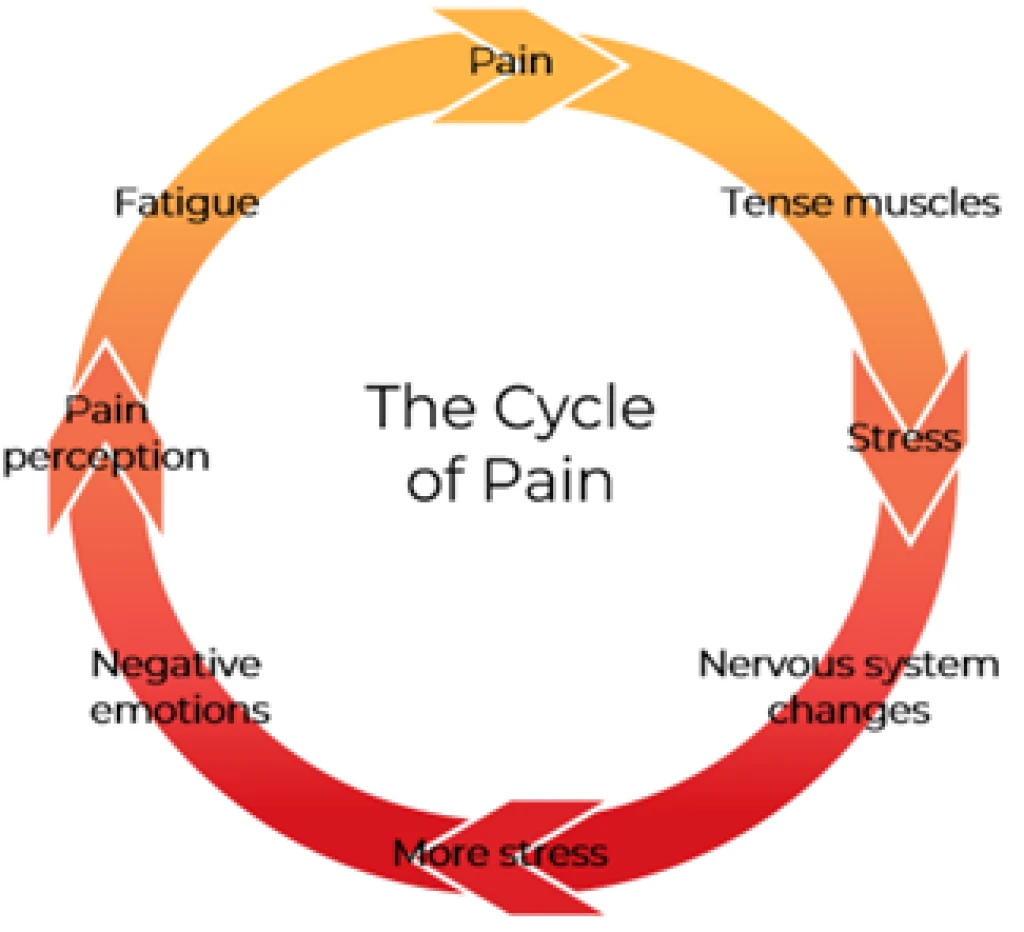
Roisin uses ‘’the cycle of pain’’, a bio-psycho-social model, to explain how living with a chronic pain condition can feel like one problem leading to another, which can make you feel trapped in a vicious cycle.